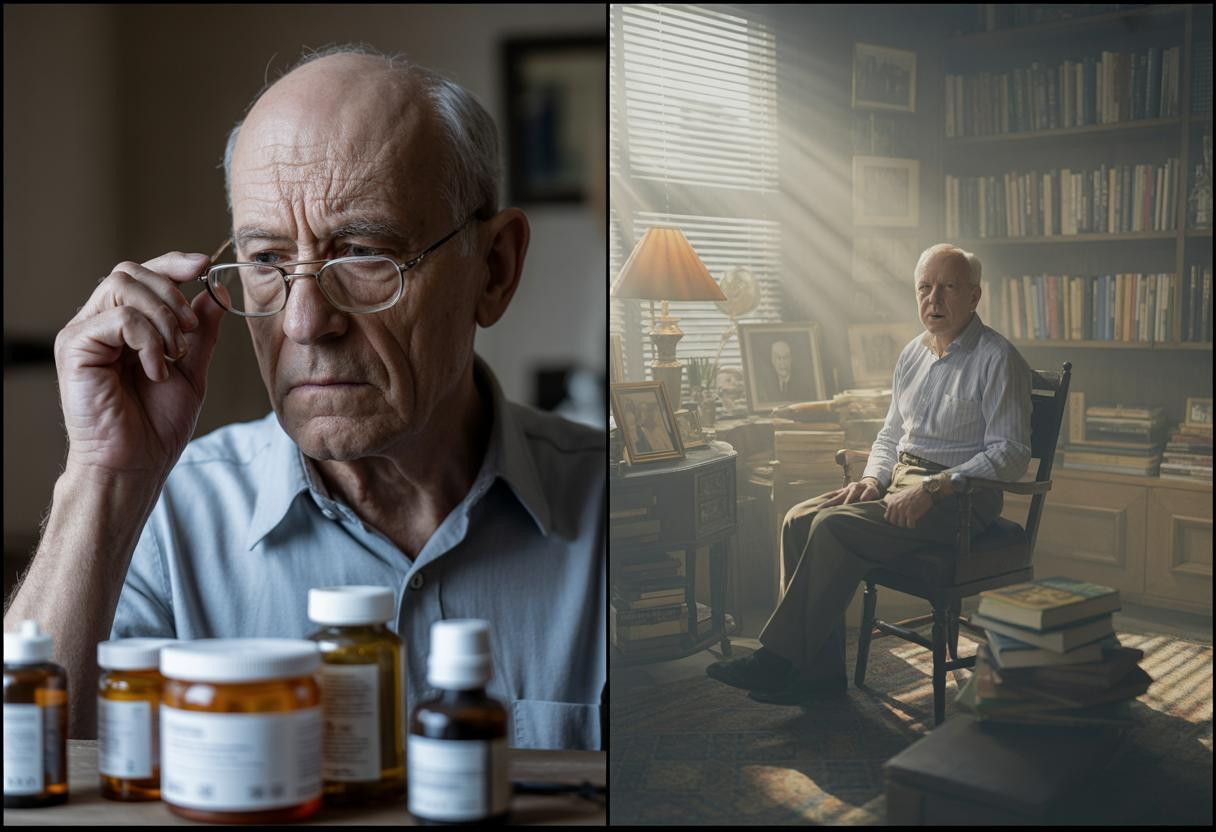
Recent groundbreaking research has uncovered an alarming connection between three widely prescribed antidepressants and long-term memory decline. This discovery has sent ripples through the medical community, challenging conventional wisdom about medications that millions rely on daily. The findings suggest that what helps our mood today might be silently compromising our cognitive health tomorrow.
The troubling trio: Which antidepressants are implicated?
The 2025 BMC Medicine study identified escitalopram (Lexapro), citalopram (Celexa), and sertraline (Zoloft) as the primary culprits. These selective serotonin reuptake inhibitors (SSRIs) showed direct correlation with accelerated cognitive decline, particularly in patients with existing dementia conditions.
“What we’re seeing is particularly concerning with escitalopram, which demonstrated the fastest rate of cognitive decline among all antidepressants studied,” explains Dr. Sarah Mendelson, neuropsychiatrist at Columbia University. “These medications are like double-edged swords – they lift the fog of depression but may simultaneously be eroding memory foundations.”
How these medications affect your brain
The relationship between these antidepressants and memory resembles a borrowing system with compound interest – you get mental relief today, but potentially pay cognitive penalties for years to come. The research revealed a troubling dose-response relationship: higher medication doses consistently produced more severe memory impairments.
“Depression itself increases dementia risk by approximately twofold, creating a challenging clinical dilemma,” notes Dr. James Harrington, geriatric psychiatrist. “We’re now forced to balance immediate psychological relief against potential long-term cognitive costs.”
Warning signs you shouldn’t ignore
Memory changes while taking these medications aren’t always immediately obvious. Watch for these subtle indicators:
- Increasing difficulty recalling recent conversations or events
- Growing reliance on notes and reminders for daily tasks
- Confusion about previously familiar processes or routines
- Struggling to learn and retain new information
The gender gap in vulnerability
Surprisingly, men with dementia experienced significantly steeper cognitive decline than women when taking these medications. This gender disparity adds another layer to treatment considerations, suggesting biological differences in how these drugs interact with male and female brains.
This finding mirrors patterns seen with daily painkillers linked to dementia signs, where gender differences also emerged in vulnerability to cognitive side effects.
Practical steps if you’re currently taking these medications
If you’re currently taking one of these antidepressants, consider these important actions:
- Never stop medication without consulting your healthcare provider
- Discuss cognitive monitoring options at your next appointment
- Consider regular memory assessments to track potential changes
- Explore alternative depression treatments with fewer cognitive risks
The digital health connection
Emerging technologies like those in China’s first AI hospital and Google’s AI wearable health monitoring could revolutionize how we balance depression treatment with cognitive protection. These tools might eventually offer personalized medication management based on real-time cognitive monitoring.
Financial implications for aging Americans
The cognitive impact of these medications creates potential financial vulnerabilities similar to those discussed in retirement calculations showing faster savings depletion. Memory decline can compromise financial decision-making ability, potentially placing retirement security at risk.
Like our phones listening to conversations, these medications may be silently gathering cognitive tolls without our awareness. The challenge now becomes finding depression treatments that help without harming our future cognitive health.